Cervical Spondylotic Myelopathy: Surgical Treatment Options
When symptoms of cervical spondylotic myelopathy (CSM) persist, or worsen despite nonsurgical treatment, your doctor may recommend surgery.
The goal of surgery is to relieve symptoms by "decompressing," or relieving pressure on, the spinal cord. This involves removing the pieces of bone or soft tissue (such as a herniated disk) that may be taking up space in the spinal canal. This relieves pressure by creating more space for the spinal cord.
Candidates for Surgery
Candidates for surgery include patients who have progressive neurologic changes with signs of severe spinal
cord compression or spinal cord swelling. These neurologic changes may include:
- Weakness in the arms or legs
- Numbness in the hands
- Fine motor skill difficulties
- Imbalance issues
- Gait changes
Patients with severe or disabling pain may also be helped with surgery.
Patients who experience better outcomes from cervical spine surgery often have these characteristics:
- Younger age
- Shorter duration of symptoms
- Single, rather than multiple, areas of spinal cord involvement
- A larger area available for the spinal cord
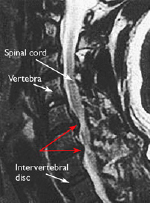
This MRI image shows herniated disks pressing on the spinal cord (red arrows), a common cause of CSM. Reproduced from Boyce R, Wang J: Evaluation of neck pain, radiculopathy and myelopathy: imaging, conservative treatment, and surgical indications. Instructional Course Lectures 52. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2003, pp.489-495.
Surgical Procedures
The four surgical procedures commonly performed to treat CSM are:
- Anterior Cervical Discectomy and Fusion
- Anterior Cervical Corpectomy and Fusion
- Laminectomy
- Laminoplasty
The procedure your doctor recommends will depend on several factors, including your overall health and the type and location of your problem.
Depending on the procedure, surgery for CSM is performed either from the front of the neck (anterior) or the back (posterior). In some cases, both anterior and posterior approaches may be necessary to address spinal cord compression and instability. Each approach has advantages and disadvantages, as shown in the table below. Your doctor will talk with you about which approach is best in your case and about the risks and benefits of surgery.
Spinal Fusion
Whether an anterior or posterior approach is used, procedures for CSM often include spinal fusion to help stabilize the spine. Spinal fusion is essentially a "welding" process. The basic idea is to fuse together the vertebrae so that they heal into a single, solid bone.
Fusion eliminates motion between the degenerated vertebrae and takes away some spinal flexibility. The theory is that if the painful spine segments do not move, they should not hurt. The degree of limitation that you experience will depend upon how many spine segments or "levels" of your spine were fused.
All spinal fusions use some type of bone material, called a bone graft, to help promote the fusion. The small pieces of bone are placed where disk or bone has been removed. Sometimes larger, solid pieces are used to provide immediate structural support to the vertebrae.
In some cases, the doctor may implant a spacer or synthetic "cage" between the two adjoining vertebrae. This cage usually contains bone graft material to allow a spinal fusion to occur between the two vertebrae.
After the bone graft is placed or the cage is inserted, your doctor will use metal screws, plates, and rods to increase the rate of fusion and further stabilize the spine.
Bone graft sources: Bone graft material is used to fill in the space left after a disk is removed. It is also placed along the sides of the vertebrae to assist the fusion. A bone graft is primarily used to stimulate bone healing. It increases bone production and helps the vertebrae heal together into a solid bone.
The bone graft will come from either your own bone (autograft) or from a donor (allograft). If an autograft is used, the bone is usually taken from your hip area. Harvesting a bone graft requires an additional incision during your surgery. It lengthens surgical time and may cause increased pain after the operation. Your doctor will talk to you about the advantages and disadvantages of using an autograft versus an allograft.
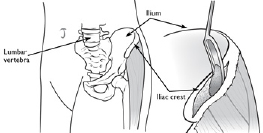
Most autografts are harvested from the iliac crest of the hip.
Anterior Approach
An "anterior" approach means that the doctor will approach your neck from the front. He or she will operate through a 1- to 2-inch incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.
Anterior cervical discectomy and fusion: During this procedure, your doctor will remove the problematic disk and any additional bone spurs, if necessary, and then stabilize the spine through spinal fusion. Typically, a plate with screws is added to the front of the spine for added stability.

Anterior cervical corpectomy and fusion: This procedure is like discectomy, except that, rather than a disk, a vertebra (bone) is removed. As in discectomy, the spine is then stabilized through spinal fusion.
In some cases, both disk and bone may be pressing on the spinal cord. In this situation, your doctor may perform a combination of discectomy and corpectomy.
Posterior Approach
A "posterior" approach means that the doctor will approach your neck from the back. He or she will make an incision along the midline of the back of the neck. Posterior approaches for decompression include laminectomy and laminoplasty. These procedures are often also accompanied by spinal fusion.
Laminectomy: In this procedure, the doctor removes the bony arch that forms the backside of the spinal canal (lamina), along with any bone spurs and ligaments that are compressing the spinal cord. Laminectomy relieves pressure on the spinal cord by providing extra space for it to drift backward.
While laminectomy ensures complete decompression of the spinal cord, the procedure makes the bones less stable. For this reason, patients who undergo laminectomy frequently require spinal fusion with a bone graft and possibly screws and rods.
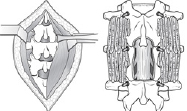
(Left) To access the spine in laminectomy, muscles are pulled back to expose the bone. (Right) After the laminectomy, bone graft material and screws are placed along the sides of the vertebrae to help with healing.
Posterior laminectomy is often recommended for people who have very small spinal canals, enlarged or swollen soft tissues at the back of the spine, or problems in more than four spine segments (levels). In a patient with a kyphotic (bent forward) spine, the spinal cord will not float or shift backward—so the doctor will often use a combined posterior and anterior approach to ensure the best outcome.

A posterior laminectomy and fusion from the front (left) and side (right).
Laminoplasty: In this alternative to laminectomy, instead of removing the bone, the lamina is thinned out on one side and then cut on the other side to create a "hinge"--much like a door. Using the hinge to open this bony area expands the space available for the spinal cord. It also allows the doctor to address adjacent spine segments, or levels, that may be mildly compressed.
Laminoplasty preserves from 30 to 50 percent of motion at the involved levels of the spine. This is a greater percentage than either laminectomy or anterior surgery. Since neck pain is often related to motion—and some motion remains after the procedure—laminoplasty is not usually used to treat patients with neck pain.
While laminoplasty increases the space available, the procedure does not ensure that the spinal canal will be completely open for the spinal cord. Another disadvantage is that, in some cases, the lamina that is hinged can inadvertently close.
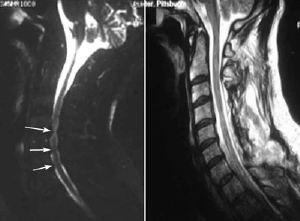
Left) This MRI shows both anterior and posterior spinal cord compression (arrows). (Right) An MRI of the same patient after laminoplasty shows increased space in the spinal canal. Reproduced from Cornett CA, Braly BA, Kang J, Donaldson, WF: Laminectomy and fusion and laminoplasty: indications and techniques. Orthopaedic Knowledge Online Journal 2012; 10(1). Accessed July 2015.
Combined Approach
Some patients will require combined anterior and posterior approaches to ensure the best outcome. This includes patients who have:
- Fixed or severe kyphosis (abnormal cervical spine curvature)
- Severe osteoporosis that has weakened the bone
- Multiple levels of involvement requiring supplemental stabilization
|
Advantages |
Disadvantages |
|
|
Anterior Approach |
• Good relief of neck pain • Spine is stabilized with fusion • Restores alignment of the spine • Direct removal of problem structures |
• Anterior approach complications • Bone graft complications • Loss of motion • Swallowing difficulty or hoarseness |
|
Advantages |
Disadvantages |
|
|
Posterior Approach |
• Less motion loss (laminoplasty) • May address more spine levels • Avoids bone graft complications |
• Wound complications • Indirect decompression • Cannot be used for kyphotic spines • Late instability or deformity (laminoplasty) • Inconsistent relief of neck pain (laminoplasty) |
Complications
As with any surgery, there are risks associated with cervical spine surgery. Possible complications can be related to the approach used, the bone graft, healing, or long-term changes. In general, elderly patients have higher rates of complications from surgery. And so, do patients who are overweight, smokers, and patients with diabetes or multiple medical problems.
Before your surgery, your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications.
General Risks
The potential risks and complications for any cervical spine surgery include:
- Infection
- Bleeding
- Nerve injury
- Spinal cord injury
- Reaction to anaesthesia
- The need for additional surgery in the future
- Failure to relieve symptoms
- Tear of the sac covering the nerves (dural tear)
- Life-threatening medical problems, such as heart attack, lung complications, or stroke
Anterior Cervical Spine Surgery Risks
The potential risks and complications of anterior cervical spine surgery include:
- Soreness or difficulty with swallowing
- Voice changes
- Difficulty breathing
- Injury to the oesophagus
- Degeneration of disk levels above or below the surgery level
Additional risks and complications of anterior cervical discectomy and spinal fusion include:
- Misplaced, broken, or loosened plates and screws
- Complications relating to the bone graft, including hip pain (if an autograft is used), dislodgement, fracture, or severe settling
- Non-union of the spinal fusion
Posterior Cervical Spine Surgery Risks
The potential risks and complications of posterior cervical spine surgery include:
- Degeneration of disk levels above or below surgery level
- Injury to the vertebral artery
- Stretch on the nerves from the spinal cord drifting backwards
- Wound breakdown
Recovery
After surgery, you will typically stay in the hospital for 1 or 2 days. This will vary, however, depending on the type of surgery you have had and how many disk levels were involved. Most patients can walk and eat on the first day after surgery.
Depending on the procedure you have had, a drain may be placed in your spine to collect any fluid or blood that may remain after surgery.
It is normal to have difficulty swallowing solid foods for a few weeks or have some hoarseness following anterior cervical spine surgery. For this reason, your doctor may prescribe antacids or recommend that your diet include softer foods--such as soup or milkshakes-in the early postoperative period.
You may need to wear a soft or a rigid collar at first. How long you should wear it will depend on the type of surgery you have had.
Discharge Instructions
When you are discharged, your doctor will give you specific instructions to follow at home. These instructions will vary depending on the type of procedure you have had. Discharge instructions after surgery may include:
- Time spent walking or sitting in a chair is unlimited.
- Contact your doctor if you see signs of infection. Signs of infection include:
- Persistent fever (higher than 101.5 degrees)
- Shaking chills
- Increased redness, tenderness, or swelling of your wound
- Drainage from your wound
- Increasing pain with both activity and rest
- Your staples or sutures can be removed at the follow-up office visit around two weeks after surgery.
- Do not take anti-inflammatory medication for six weeks following surgery.
- Do not lift anything greater than 10-15 lbs.
- Do not drive a car until cleared by your doctor.
After spinal fusion, it may take from 6 to 12 months for the bone to become solid. For this reason, your doctor may give you additional restrictions to follow. For example, right after your operation, your doctor may
recommend only light activity, like walking. As you regain your strength, you will be able to slowly increase your
activity level.
New Symptoms
Depending on the extent of your surgery and the number of spine levels fused, you may notice some neck stiffness or loss of motion after your procedure. Also, as nerves begin to awaken following surgery, you may experience different nerve symptoms or feelings than you had before. This is normal and will often continue to improve for 1 to 2 years after surgery.
If your nerve symptoms and pain get progressively worse, or if you have any problems with infection or wound healing, contact your doctor.
Physical Therapy
Usually by 4 to 6 weeks, you can gradually begin to do range-of-motion and strengthening exercises. Your doctor may prescribe physical therapy during the recovery period to help you regain full function.
Return to Work
Most people can return to a desk job within a few days to a few weeks after surgery. They may be able to return to full activities by 3 to 4 months, depending on the procedure. For some people, healing may take longer.
Outcomes
Regardless of the approach used, the desired outcome of surgery is to stabilize the spine and prevent neurologic problems from worsening. A secondary goal is to potentially improve neck pain—as well as the motor, sensory, and other neurological symptoms that may be present. The goal of surgery is not necessarily to restore normal function.
Outcomes will vary from patient to patient. Typically, with respect to pre-surgical symptoms, one-third of patients improve, one-third stay the same, and one-third continue to worsen over time. In most cases, the symptoms a patient is experiencing before surgery will be like those that he or she will have following surgical intervention. Your doctor will discuss this with you and provide information on the likelihood of improvement in your specific situation.













