Lumbar Spinal Stenosis
Table of Contents
Introduction
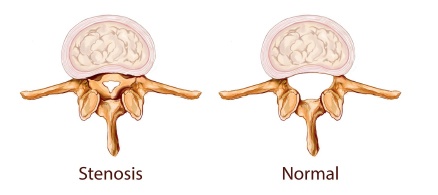
Spinal stenosis describes narrowing inside the spinal canal and mainly occurs from a combination of aging and degenerative changes in the spine. Wear and tear on the parts of the spine can cause discs to bulge, spine ligaments to thicken, and joints near the spinal canal to become enlarged. These can take up space inside the spinal canal and put pressure on the spinal nerves. Changes like these mostly affect people over 60 years of age. However, spinal stenosis also occurs in younger people who have abnormally small spinal canals from birth. Spinal stenosis usually causes back pain and leg pain that comes and goes with activities, such as walking.
Learn about lumbar spinal stenosis including
- what part of the spinal anatomy is affected
- what symptoms are present
- how the condition is diagnosed
- what treatment options are available
Anatomy
Stenosis can occur in all areas of the spine, but it is most common in the lumbar spine. To understand your symptoms and treatment choices, it helps to start with a basic understanding of the anatomy of your low back. This includes becoming familiar with the various parts that make up the lumbar spine and how these parts work together.
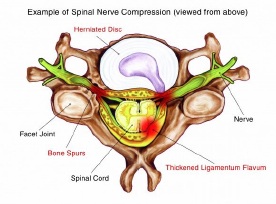
The spinal canal is a tube within the bones of the spinal column. The spinal cord and spinal nerves are normally protected inside this bony tube. Bordered by bone and tough ligaments, the spinal canal cannot expand when something crowds the space within the canal. Normally there is space between the spinal cord and the edges of the surrounding spinal canal.
Causes
Anything that places the spinal cord and spinal nerves at risk. The lack of space puts pressure on them, causing irritation and inflammation. Conditions that can narrow the spinal canal include infection, tumours, trauma, herniated discs, arthritis, thickening of ligaments, and bone spurs.
Spinal stenosis usually occurs in older people due to years of wear and tear (degeneration) of the spine. The changes that happen from this process include thickened ligaments, bone spurs, facet joint enlargement (hypertrophy), and bulging discs.
In some cases, simply bending over relieves the symptoms. This makes the spinal canal larger and provides more space so that the blood flow to the spinal nerves increases. Activities that increase the demand for blood flow cause the blood vessels to swell and enlarge. If there is no room for this to occur, the blood flow cannot increase. This causes pain and weakness because the nerves cannot get enough oxygen to meet the demand.
Some people have a narrow spinal canal from birth. This does not mean they automatically feel symptoms of stenosis. But if the spinal canal is too narrow, it can lead to pressure on the spinal nerves. People who have a very narrow canal are at risk for stenosis because even minor crowding inside the spinal canal can lead to symptoms.
Symptoms
The main symptoms of spinal stenosis are felt in the legs-heaviness, weakness, and pain with walking or prolonged standing. The symptoms are caused by the nerve roots getting squeezed, which upsets the normal signals traveling from the brain to the body. Irritation of the nerves is worse when standing or walking due to pressure and stretching of the nerves. Symptoms often disappear with rest. Sitting down seems to take pressure of the nerve roots.
Diagnosis
Diagnosing a herniated nucleus pulposus begins with a complete history of the problem and a physical exam.
You may be asked to take a variety of diagnostic tests. The tests are chosen based upon what the physician suspects is causing your pain. The most common diagnostic tests to determine whether you have spinal stenosis are X-rays of your lower back and an MRI scan. In some cases, a CT scan may be ordered, either in addition to an MRI or instead of one.
X-rays
An X-ray is a process that uses radioactive materials to take pictures of bone. If the doctor suspects vertebral degeneration, X-rays can be used to verify: a decrease in the height of space between discs, bone spurs, nerve bundle sclerosis (hardening), facet hypertrophy (enlargement), and instability during flexion or extension of limbs. X-rays show bones, but not much soft tissue. They will be used if fractures, infections, or tumours are suspected.
MRI
An MRI can be used to verify loss of water in a disc, facet joint hypertrophy (enlargement), stenosis (narrowing of spinal canal), or a herniated disc (protrusion or rupture of the intervertebral disc).
CT Scan
The CT scan is an X-ray test that can show both bones and soft tissues. The scan forms a set of cross-sectional images that can show disc problems and degeneration of bones, such as bone spur formation or facet hypertrophy (enlargement). CT scan images are not as clear as either X-rays or an MRI. To make the soft tissues easier to see, the CT scan is often combined with a myelogram.
Other tests are sometimes used to make sure there are not additional problems causing your back pain.
Treatment Options
Conservative Treatment
On your first visit to a back specialist, the initial determination that must be made is the seriousness of the problem. Some problems need immediate attention-possibly even surgery. The clear majority of back problems do not require surgery. Spinal stenosis is a slowly progressive back problem that may respond to conservative care.
A variety of treatment options exists for spinal stenosis. In most cases, simple therapies such as mild pain medications and rest are effective in relieving the immediate pain. Physical therapy may be beneficial if symptoms are not relieved with simple measures. The overall goal of treatment is to make you as comfortable as soon as possible, and to get you back to normal activity in a timely manner.
Medications
Mild pain medications can reduce pain when taken properly. The medications will not cure or stop the progression of the problem, but they will help with pain control.
Physical Therapy
If your condition is causing only mild symptoms and does not appear to be getting worse, your doctor may have you work with a physical therapist. A well-rounded rehabilitation program assists in calming pain and inflammation, improving your mobility and strength, and helping you do your daily activities with greater ease and ability.
Positions, movements, and exercises are prescribed to reduce pain. Treatments may also include lumbar traction to gently stretch the low back, easing pressure on the spinal nerves. Exercises are used to improve cardiovascular fitness and to tone the low back and abdominal muscles. Therapy sessions may be scheduled two to three times each week for up to six weeks.
The goals of physical therapy are to help you
- Learn to manage your condition and control symptoms
- Learn correct posture and body movements to reduce back pain
- Maximize flexibility and core strength
- Foster heart and lung fitness
ESI
An epidural steroid injection (ESI) can be used to relieve the pain of stenosis and irritated nerve roots, as well as to decrease inflammation. Injections can help reduce swelling from inflamed tissues in the spinal canal, which may result in less irritation on the nerves. The steroid injections are a combination of cortisone (a powerful anti-inflammatory steroid) and a local anaesthetic that are given through the back into the epidural space. Epidural steroid injections are not always successful in relieving symptoms of inflammation. They are only used when conservative treatments have failed.
Surgical Treatment
Spinal stenosis may continue to get worse over time. Surgery may be considered as a treatment option if
- You experience an increase in the weakness in your legs
- You can no longer walk without leg pain
- You begin to have trouble controlling your bowels or bladder
- The pain becomes unbearable
Because spinal stenosis is more common in elderly people, one of the considerations for suggesting surgery is the overall physical condition of the patient. Back surgery is a major undertaking. If you have serious medical problems, the risks may be too great to have spine surgery. The decision is jointly made with your surgeon and your regular medical doctor.
The main goal of any surgical procedure used to treat spinal stenosis is to remove the pressure on the nerve roots in the lumbar spinal canal. This means that the tube of the spinal canal must be made larger, and any bone spurs that are pushing into the nerve roots must be removed. This type of surgical procedure is usually called a decompression of the lumbar spine, or a decompressive laminectomy of the lumbar spine.
To free up or "decompress" the nerves, the surgeon must remove a section of bone from the back of the spine (lamina). The surgeon may also have to remove a portion of the facet joints. The lamina and facet joints normally provide stability in the spine. Removal of either or both can cause the spine to become loose and unstable. When this occurs, doctors will include fusion as part of the procedure. Likewise, patients with spinal instability who need surgery for spinal stenosis will likely also need lumbar fusion.













