Cervical Stenosis
Table of Contents

Introduction
Most cervical problems are due to degenerative changes that occur in the discs and joints of the neck. Degenerative changes that affect the structures of the spine can cause the spinal canal to become too narrow, a condition called spinal stenosis. This may lead to pressure on the spinal cord. Bone spurs that stick into the spinal canal take up space, making the spinal canal smaller. They can press against the spinal cord or nerve roots.
Pressure on the spinal cord from spinal stenosis can cause symptoms of myelopathy. Myelopathy may impair normal walking, hand and finger use, and bowel and bladder function. Doctors take these symptoms very seriously because severe myelopathy that is not treated may lead to permanent nerve or spinal cord damage.
Pressure on nearby nerve roots can cause radiculopathy and may produce pain, weakness, or sensory changes in the area supplied by nerves that go from the cervical spine to the shoulder, arm, or hand.
Learn about cervical spinal stenosis including
- What causes the condition
- What symptoms are present with spinal stenosis
- How the condition is diagnosed
- What treatment options are available
Anatomy
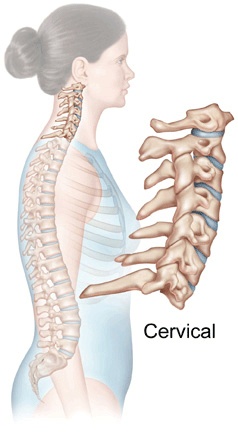
In order to understand your symptoms and treatment choices, it is helpful to start with a basic understanding of the anatomy of the neck. This includes becoming familiar with the various parts that make up the cervical spine and how they work together.
Learn more about the anatomy of the cervical spine.
Causes
To best understand cervical spinal stenosis, it is helpful to know how wear and tear affects the parts of the spine. This process is called degeneration.
As we age, the disc loses some of its water content and, as a result, some of its shock absorbing ability. The first changes that occur in the disc are tears in the outer ring of the disc, called the annulus. Tears in the annulus may occur without symptoms. You may not notice when they occur or what caused them. These tears heal by forming scar tissue.
Scar tissue is weaker than normal tissue. Repeated injuries and tears cause more wear and tear to the disc. As the disc wears, it gets less and less "spongy", eventually becoming unable to act as a shock absorber.
As the disc continues to wear, it begins to collapse. The space between each vertebra becomes smaller. This collapse affects how the facet joints in the back of the spine "line up." Like any other joint in the body, the change in the way the spine bones fit together causes abnormal pressure on the articular cartilage covering the facet joints. Articular cartilage is a smooth, shiny material that covers the end of the bones in most joints in the body. Over time, this abnormal pressure causes wear and tear arthritis (osteoarthritis) of the facet joints.
Bone spurs may form around the vertebrae and facet joints. Eventually, bone spurs may begin to form. These spurs may begin to press against the spinal cord, leading to the symptoms of myelopathy discussed earlier. Or the spurs can put pressure on the nerves where they leave the spinal canal. This can lead to symptoms of radiculopathy (described below).
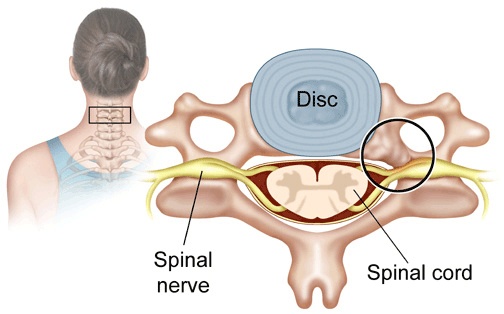
The combined effects of the bone spurs, bulging discs, and thickened ligaments place the spinal cord at risk of being squeezed inside the spinal canal.
Symptoms
The symptoms from spinal stenosis depend on whether pressure is affecting the spinal nerve roots or the spinal cord. A " pinched " nerve in the neck (radiculopathy) usually only causes symptoms in the neck and arms. Pressure on the spinal cord (myelopathy) can affect the arms and legs.
Radiculopathy is a condition that can happen from pressure on a spinal nerve root. Commonly thought of as a "pinched nerve," this type of pressure feels different than pressure on the spinal cord. Pressure on an irritated or inflamed nerve root may produce feelings of pins and needles in the area supplied by the nerve root. The pain may feel deep, dull, and achy. Or you may have sharp, shooting pain along the path of the nerve. Muscles controlled by the affected nerve root may also weaken. Muscles controlled by the affected nerve root may also weaken.
Pressure on the spinal cord (myelopathy) is a greater concern, because it can lead to permanent spinal cord damage. Symptoms from myelopathy vary. Feelings of numbness or weakness can affect both arms and both legs. A loss of muscle control in the legs, called spasticity, may cause difficulty walking. "Position sense" may be lost in the arms or legs. This affects the ability to know where your arms or legs are when your eyes are closed. When this occurs, it becomes difficult to use the arm and hands and to know where you are placing your feet as you walk. Myelopathy may disturb the normal function of the bowels and bladder.
Diagnosis
Finding the cause of your neck problem begins with a complete history and physical exam. After the history and physical exam, your doctor will have a good idea of the cause of your pain and symptoms. To make sure of the exact cause of your neck pain, several diagnostic tests can be used. Standard X-rays, taken in the doctor's office, are usually a first step in considering any neck problem and will give your doctor an idea of whether cervical spinal stenosis exists. These include an oblique (angled) view, along with X-rays taken as you bend forward (flexion) and backward (extension). Your doctor will also determine whether other tests, such as an MRI, are needed.
X-rays of cervical disc degeneration. (Click on images to enlarge.)



MRI scan showing cervical stenosis. (Click on image to enlarge.)

Treatment Options
Conservative Treatment
Epidural Steroid Injection (Nerve Block)
If other treatments do not relieve your neck pain, you may be given an epidural steroid injection (ESI), also called a nerve block. An ESI places a small amount of cortisone into the bony spinal canal. Cortisone is a strong anti-inflammatory medicine that may control the inflammation surrounding the nerves and may ease the pain caused by irritated nerve roots. This injection is often used when other conservative measures do not work, or to postpone surgery. This treatment is not always successful but may provide short-term help.
Physical Therapy
If your condition is causing only mild symptoms and does not appear to be getting worse, your doctor may have you work with a physical therapist. A well-rounded rehabilitation program assists in calming pain and inflammation, improving your mobility and strength, and helping you do your daily activities with greater ease and ability.
In mild cases, nonsurgical treatments offer ways to control symptoms and enable you to improve without surgery. You may be issued a neck brace to hold your neck steady, reducing extra strain. You will need to limit your activities, especially heavy and repeated movements of the arms and neck. Therapists use electrical stimulation to ease muscle spasm and pain. Treatments may also include cervical traction to gently stretch the joints and muscles in the neck. Therapy sessions may be scheduled two to three times each week for up to six weeks.
The goals of physical therapy are to help you
- learn correct posture and body movements to minimize the effects of stenosis
- maintain appropriate activity levels
- identify symptoms of stenosis that require medical attention
- learn ways to manage your condition
Surgical Treatment
Cervical myelopathy can be a serious problem. The pressure on the spinal cord usually will not go away without surgery, and the symptoms may continue to get worse. If you do not improve with non-operative care, your doctor may suggest surgery.
There are several surgical procedures used to treat cervical spinal stenosis that is causing cervical myelopathy; all have the same goal-to relieve the pressure on the spinal cord by making the spinal canal larger.
Your surgeon may suggest an operation called a laminectomy, in which the backside of the vertebrae is opened to allow more room for the spinal cord. Discectomy, the removal of one or more discs, may be suggested if stenosis is coming from problems of disc herniation. This surgery may be done from the front or back of the spine. Or your surgeon may suggest an operation that is done from the front of the neck - a corpectomy and strut graft. This operation involves removing the discs and vertebral bodies in the area where problems are occurring. Bone spurs that are pushing into the spinal cord are also removed. The vertebrae are then replaced with a solid piece of bone graft (called a strut graft). The strut graft heals over time to create a solid fusion of the spine where the vertebral bodies have been removed.













