Lumbar Herniated Disc
Table of Contents
Introduction
It's common to hear the terms "ruptured disc" and "slipped disc." People often assume that everyone who has back pain has a ruptured disc. However, a true herniated nucleus pulposus (the medical name for this problem) is not very common.
Learn about herniated discs including
- What a herniated disc really is?
- How it causes problems?
- How the condition is diagnosed?
- What treatment options are available?
Anatomy
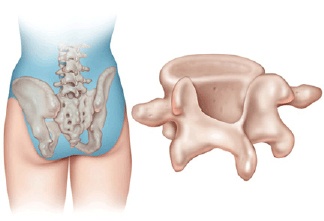
To understand your symptoms and treatment options, it helps to begin with an understanding of the anatomy of your low back. This includes becoming familiar with the various parts that make up the lumbar spine and how these parts work together.
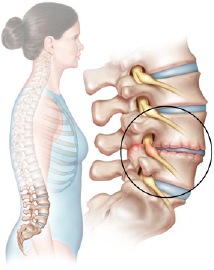
The intervertebral discs are the shock-absorbing cushions between each vertebra of your spine. There is one disc between each vertebra. Each disc has a strong outer ring of fibres, called the annulus, and a soft, jelly-like centre, called the nucleus pulposus.
The annulus is the disc's outer layer and the strongest area of the disc. The annulus is a strong ligament that helps connect each vertebra together. The nucleus in the centre of the disc serves as the main shock absorber.
A herniated disc occurs when the intervertebral disc's outer fibres (the annulus) are damaged and the soft inner material of the nucleus pulposus ruptures out of its normal space. If the annulus tears near the spinal canal, the nucleus pulposus material can push into the spinal canal.
Causes
A true herniated nucleus pulposus is most common in young and middle-aged adults. It rarely occurs in children. Degenerative changes in the spine that occur with aging make it less likely to develop a true herniated disc. This is because the nucleus in the middle of the disc dries out, making it less likely to squeeze out of the disc.
Discs can rupture suddenly because of too much pressure all at once. For example, falling from a ladder and landing in a sitting position can cause a great amount of force through the spine. If the force is strong enough, either a vertebra can break or a disc can rupture. Bending places high forces on the discs between each vertebra. If you bend and try to lift something that is too heavy, the force can cause a disc to rupture.
Discs can also rupture from a small amount of force, usually due to weakening of the annulus from repeated injuries that add up over time. As the annulus becomes weaker, at some point lifting or bending causes too much pressure across the disc. The weakened disc ruptures while doing something that five years earlier would not have caused a problem. This is because of aging on the spine-the most common reason for a disc herniation in the lumbar spine.
A herniated disc causes problems in two ways. First, the material that has ruptured into the spinal canal from the nucleus pulposus can cause pressure on the nerves in the spinal canal. There is also some evidence that the nucleus pulposus material causes a chemical irritation of the nerve roots. Both the pressure on the nerve root and the chemical irritation can lead to problems with how the nerve root functions. The combination of the two can cause pain, weakness, and numbness in the area of the body to which the nerve supplies sensation.
Symptoms
The symptoms of a true herniated disc may not include back pain at all. The symptoms come from pressure on, and irritation of, the nerves. But many people do have back pain because they have other problems in their back when the disc ruptures. The symptoms of a herniated disc usually include:
- Pain that travels into one or both legs
- Numbness or tingling in areas of one or both legs
- Muscle weakness in certain muscles of one or both legs
- Loss of the reflexes in one or both legs
Where these symptoms occur depends on which nerve(s) has been affected in the lumbar spine. Therefore, the location of the symptoms helps determine your diagnosis. Knowing where the pain is perceived gives your doctor a better idea of which disc has probably ruptured.
Diagnosis
Diagnosing a herniated nucleus pulposus begins with a complete history of the problem and a physical exam.
Your doctor will want to make sure that you are aware when you must urinate or have a bowel movement. If there is a problem, it could indicate that a herniated disc in the lumbar spine is pushing against the spinal cord.
Diagnostic Tests
X-rays
The doctor may suggest taking X-rays of your low back. Regular X-rays can't show a herniated disc, but they can give your doctor an idea of how much wear and tear is present in the spine.
MRI
The MRI scan is the most common test used to diagnose a herniated disc. This test is painless and accurate. There do not appear to be any side effects with the test. MRI has almost completely replaced other tests when a herniated disc is suspected.
CT Scan
Sometimes the X-ray and MRI do not tell the whole story. Other tests may be suggested. A myelogram, usually combined with a CT scan, may be necessary to give as much information as possible.
Discogram
When surgery for lumbar disc herniation is being considered, doctors may order a discogram to locate which discs are causing pain.
EMG and SSEP
Electrical tests can confirm that the pain in your leg is coming from a damaged nerve. These tests may be required before a decision is made to proceed with surgery.
Treatment Options
Conservative Treatment
The treatment of a herniated disc depends on the symptoms. If the symptoms are getting better, your doctor may suggest watching and waiting to see if they go away. If they are getting steadily worse, your doctor may be more likely to suggest surgery. Many people, who initially have problems due to a herniated disc, find their symptoms completely resolve over several weeks or months.
Observation
You may not need any treatment other than watching to make sure that the problem does not progress. If the pain is bearable and symptoms from nerve or spinal cord pressure are not getting worse, your doctor may just want to watch and wait.
Pain medications
Depending on the severity of your pain, medications can be used to help control it. Over-the-counter pain relievers, such as ibuprofen, Tylenol(tm), and some of the newer anti-inflammatory medications, may be helpful. Make sure to follow the directions and not take too many.
If these types of medications do not control the pain, your doctor may prescribe stronger pain pills narcotic or non-narcotic pain medications. Narcotic pain medications are very strong but also very addictive. Non-narcotic pain medications are less addictive, but are somewhat less effective than narcotics. Most physicians do not like to prescribe narcotics for more than a few days or weeks.
Rest
If the pain is more severe, it may be necessary to take a few days off from work and decrease your activities. Your doctor may also prescribe a back brace to help limit movement around the injured disc. After two days, you should begin to get moving. Start with a gentle walking program and increase the distance you walk each day.
Physical Therapy
Patients with a herniated disc are commonly prescribed physical therapy. A well-rounded rehabilitation program assists in calming pain and inflammation, improving your mobility and strength, and helping you do your daily activities with greater ease and ability.
Therapy visits are designed to help control symptoms, enabling you to resume normal activities. Exercises focus on improving strength and coordination of the low back and abdominal muscles. The emphasis of therapy is to help you learn to take care of your back through safe exercise and selfcare when symptoms flare up. Therapy sessions may be scheduled two to three times each week for up to six weeks.
The goals of physical therapy are to help you
- Learn ways to manage your condition and control symptoms
- Resume appropriate activity levels
- Learn correct posture and body movements to reduce back strain
- Maximize your flexibility and strength
Epidural Steroid Injection (ESI)
The ESI is usually reserved for more severe pain from nerve root irritation due to a herniated disc. It is not usually suggested unless surgery is fast becoming an option. An ESI is only successful in reducing the pain from a herniated disc in about half the cases.
Surgical Treatment
Surgical treatment for a herniated disc depends on several factors such as your specific problem and your surgeon's experience.
- Laminotomy and Discectomy
- Microdiscectomy
- Endoscopic Discectomy
Complications
Like all surgical procedures, operations on the back may have complications. Because the surgeon is operating around the spinal cord, back operations are always considered extremely delicate and potentially dangerous. Take time to review the risks associated with lumbar spine surgery with your doctor. Make sure you are comfortable with both the risks and the benefits of the procedure planned for your treatment.













