Idiopathic Scoliosis in Children and Adolescents
Scoliosis is a condition that causes the spine to curve sideways. There are several different types of scoliosis that affect children and adolescents. By far, the most common type is "idiopathic," which means the exact cause is not known.
Most cases of idiopathic scoliosis occur between age 10 and the time a child is fully grown. Scoliosis is rarely painful—small curves often go unnoticed by children and their parents, and are first detected during a school screening or at a regular check-up with the paediatrician.
In many cases, scoliosis curves are small and do not require treatment. Children with larger curves may need to wear a brace or have surgery to restore normal posture.
Description
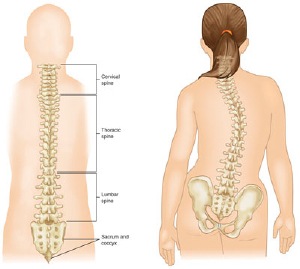
Scoliosis causes the bones of the spine to twist or rotate so that instead of a straight line down the middle of the back, the spine looks more like the letter "C" or "S." Scoliosis curves most commonly occur in the upper and middle back (thoracic spine). They can also develop in the lower back, and occasionally, will occur in both the upper and lower parts of the spine.
Idiopathic scoliosis curves vary in size, and mild curves are more common than larger curves. If a child is still growing, a scoliosis curve can worsen rapidly during a growth spurt.
Although it can develop in toddlers and young children, idiopathic scoliosis most often begins during puberty. Both boys and girls can be affected, however, girls are more likely to develop larger curves that require medical care.
Other less common types of scoliosis include:
- Congenital scoliosis. Problems in the spine sometimes develop before a baby is born. Babies with congenital scoliosis may have spinal bones that are not fully formed or are fused together.
- Neuromuscular scoliosis. Medical conditions that affect the nerves and muscles, such as muscular dystrophy or cerebral palsy, can lead to scoliosis. These types of neuromuscular conditions can cause imbalance and weakness in the muscles that support the spine.
Cause
Although doctors do not know the exact cause of idiopathic scoliosis, they do know that it is not related to specific behaviours or activities — like carrying a heavy backpack or having poor posture.
Research shows that in some cases genetics plays a role in the development of scoliosis.
Symptoms
Small curves often go unnoticed until a child hits a growth spurt during puberty and there are more obvious signs, such as:
- Tilted, uneven shoulders, with one shoulder blade protruding more than the other
- Prominence of the ribs on one side
- Uneven waistline
- One hip higher than the other
Because adolescents are often self-conscious and avoid wearing form-fitting clothes, many cases of scoliosis are first detected during a school screening or regular pediatric check-up. If your paediatrician suspects scoliosis, he or she may refer you to a pediatric orthopaedic surgeon or a spinal deformity surgeon for a full evaluation and treatment plan.
Doctor Examination
Physical Examination
The standard screening test for scoliosis is the "Adam's forward bend test." During the test, your child will bend forward with feet together, knees straight and arms hanging free. Your doctor will observe your child from the back, looking for a difference in the shape of the ribs on each side. A spinal deformity is most noticeable in this position.
With your child standing upright, your doctor will also check to see if the hips and shoulders are level, and if the position of the head is centred over the hips. He or she will check the movement of the spine in all directions.
To rule out other causes of spinal deformity, your doctor will check for limb-length discrepancies, abnormal neurological findings, and other physical problems.
X-rays
X-rays will provide clear images of the bones in your child's spine. They allow your doctor to see the exact location of the curve and to measure how severe it is. In general, curves greater than 25° are considered serious enough to require treatment.
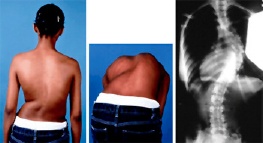
(Left) An adolescent girl with thoracic idiopathic scoliosis on the right side. (Middle) Her rib prominence is more obvious during the "Adam's forward bend test." (Right) This x-ray of her spine clearly shows the right thoracic curve. Courtesy of Texas Scottish Rite Hospital for Children
Treatment
Your doctor will consider several things when planning your child's treatment:
- The location of the curve
- The severity of the curve
- Your child's age
- The number of remaining growing years — once an adolescent is fully grown, it is not common for a curve to rapidly worsen.
By evaluating these factors, your doctor will determine how likely it is that your child's curve will worsen and be able to suggest the best treatment option.
Nonsurgical Treatment

Observation. If your child's spinal curve is less than 25° or if he or she is almost full-grown, your doctor may recommend simply monitoring the curve to make sure it does not get worse. Your doctor will recheck your child about every 6 to 12 months and schedule follow-up x-rays until your child is fully grown.
Bracing. If the spinal curve is between 25° and 45° and your child is still growing, your doctor may recommend bracing. Although bracing will not straighten an existing curve, it often prevents it from getting worse to the point of requiring surgery.
In a recent research study of scoliosis patients with curves at a high risk for worsening, bracing significantly decreased the incidence of curves that progressed to the point of needing surgery.
There are several types of braces for scoliosis. Most of them are underarm braces that are custom-made to fit your child's body comfortably. Your doctor will recommend the type that best meets your child's needs and will determine how long the brace should be worn each day.
Clothes in loose-fitting styles easily cover the brace. Your child can take off the brace for sports activities.
Surgical Treatment
Your doctor may recommend surgery if your child's curve is greater than 45°-50° or if bracing did not stop the curve from reaching this point. Severe curves that are not treated could eventually worsen to the point where they affect lung function.
A surgical procedure called "spinal fusion" will significantly straighten the curve and then fuse the vertebrae together so that they heal into a single, solid bone. This will stop growth completely in the part of the spine affected by scoliosis.
During the procedure, the spinal bones that make up the curve are realigned. Small pieces of bone — called bone graft — are placed into the spaces between the vertebrae to be fused. Over time, the bones grow together — like when a broken bone heals.
Metal rods are typically used to hold the bones in place until the fusion happens. The rods are attached to the spine by hooks, screws, and/or wires.
Exactly how much of the spine is fused depends upon your child's curve(s). Only the curved vertebrae are fused together. The other bones of the spine remain able to move and assist in motion.

(Left) This x-ray shows two large curves that require surgery. (Right) The same patient after surgery to correct the curves. Courtesy of Texas Scottish Rite Hospital for Children
Recovery
By the second day after surgery, most patients can walk without wearing a brace. Discharge from the hospital is usually less than 1 week following surgery. Most children can return to school and resume their daily activities within 4 weeks.
Long-Term Outcome
Spinal fusion is very successful in stopping the curve from growing. Surgery is also able to straighten the curve significantly, which improves the patient's appearance.
Most children can return to sporting activities within 6 to 9 months after surgery. Because surgery causes permanent limitation of some spine movements, however, participation in contact sports such as football is discouraged.
Spinal fusion does not increase the risk of complications during girls' future pregnancies or deliveries.













