Posterior Lumbar Interbody Fusion and Transforaminal Lumbar Interbody Fusion
Spinal fusion is a surgical procedure used to correct problems with the small bones in the spine (vertebrae). It is essentially a "welding" process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone.
This article focuses on just the surgical component of posterior lumbar interbody fusion and Transforaminal lumbar interbody fusion.
Interbody Fusion
Another method of fusing the lumbar spine involves removing the intervertebral disk. When the disk space has been cleared out, a metal, plastic, or bone spacer is implanted between the two adjoining vertebrae.
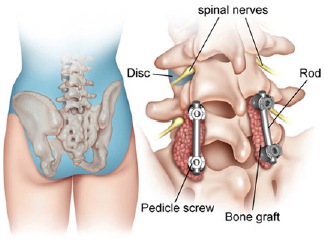
These spacers, or "cages", usually contain bone graft material. This promotes bone healing and facilitates the fusion. After the cage is inserted, surgeons often use metal screws, plates, and rods to further stabilize the spine.
An interbody fusion can be performed using a variety of different approaches.
Posterior lumbar interbody fusion (PLIF). A spacer may be inserted from the back of the spine. With this approach, your surgeon gains access to your spine by removing the bone (lamina) and retracting the nerves. Then the back of the disk can be removed and a spacer inserted.
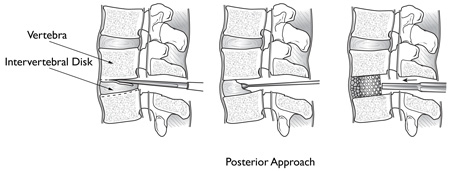
The weakened intervertebral disk is removed during a posterior lumbar interbody fusion. It is replaced with a cage, or spacer.
Transforaminal lumbar interbody fusion (TLIF). With this technique, the surgeon approaches the spine a little bit from the side. This requires less movement of the nerve roots. More recently, it has even been possible to take a direct side approach and centre the incision over the patient's flank. With this approach, the surgeon can reach the disk without moving the nerves and opening the back muscles.
Introduction
Spinal fusion is the surgical technique to stabilize the spinal bones, or vertebrae, and the disc, or shock absorber, between the vertebrae. The goal of lumbar fusion is to create solid bone between two or more vertebrae. A solid fusion between two vertebrae stops the movement between the bones. This reduces pain from motion and nerve root inflammation. Spinal fusion may be recommended for conditions such as spondylolisthesis (slippage of one vertebra over the one below), degenerative disc disease, or for recurrent disc herniation despite multiple surgeries.
Surgeons perform lumbar fusion using several techniques. The method described here is called Transforaminal lumbar interbody fusion (TLIF), an adaptation of a posterior lumbar interbody fusion (PLIF). TLIF surgery provides unilateral access to the disc space through the intervertebral foramen. Surgical Hardware called instrumentation, is applied to the spine. A special spacer, called a fusion cage, is inserted into the disc space from one side of the spine.
Bone graft material is placed into the interbody space and along the side and back of the vertebra to be fused. The surgeon will usually obtain bone graft from the patient's pelvis, although bone graft substitutes are sometimes used. These substitutes avoid having to obtain bone graft from the patient. As the bone graft heals it joins (fuses) the vertebra above and below, forming one solid bone.
TLIF provides fusion of the front and back of the lumbar spine. The front portion of the spine, called the anterior column, is stabilized by the interbody spacer and bone graft. The back portion, or posterior column, is locked in place with pedicle screws, rods and additional bone graft, alongside the backs of the vertebra.
This document will discuss:
- Anatomy of the lumbar spine
- Rationale of the TLIF operation
- Preparations for the operation by the patient
- Descriptions of the procedure
- Complications and benefits of a TLIF procedure
- Patient care after surgery
- Rehabilitation
Anatomy
The spinal column is formed by individual spine bones, called vertebrae. On the front of each vertebra is a round vertebral body. A cushion, called the intervertebral disc, sits between the vertebral bodies above and below it.
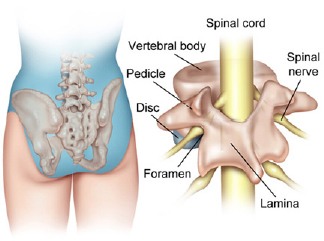
A circle of bone connects on the back of each vertebral body. The bony circle is formed by two sets of bones, the pedicle and lamina bones. The pedicles attach to the back of the vertebral body, one on the left and one on the right. The lamina bones complete the circle by connecting to each pedicle.
When the vertebrae are stacked up, the bony circles form a protective tube, called the spinal canal. The spinal canal protects the spinal cord and spinal nerves, much like the skull protects the brain.
The surgical drain is usually removed within 48 hours of the operation, and patients can usually shower by this time. When patients go home, they are usually given a prescription for oral narcotic pain medication.
In the lumbar spine, the spinal nerves that travel inside the spinal canal exit through the sides of the vertebrae. Each vertebral pair has two such passageways, one on the left and one on the right. These openings are called the foramina ("foramen" is singular).
TLIF is performed through a posterior incision over the lumbar spine. The procedure can be done with an "open exposure" or a "percutaneous exposure". A percutaneous exposure is a type of minimally invasive surgery where smaller incisions in the skin are used to perform surgery. Your surgeon will discuss with you whether your surgery can be done using the percutaneous exposure. Bone graft is usually obtained from the posterior iliac crest where there is a reservoir of bone that surgeons use for all types of bone grafting procedures.
Rationale
Lumbar fusion is indicated in patients who have failed conservative treatment and have disabling back and/or leg symptoms. Specific diagnoses include: spondylolisthesis, degenerative disc disease, and recurrent herniated disc--all leading to chronic, mechanical back pain. The TLIF procedure addresses the disc as a pain generator in causing the chronic mechanical back pain and eliminates the disc as the source of that pain. The goal of a spinal fusion operation is to obtain a solid bony union between two or more vertebrae.
Potential advantages of the TLIF procedure:
- The procedure can allow the surgeon to obtain a fusion of both the anterior portion of the spine and the posterior portion of the spine through a single posterior approach.
- The chance for a successful fusion is increased due to the larger area for bone graft placement. Bone graft can be placed both in the area behind the vertebrae, to the side of the vertebrae and in the disc space between the vertebrae.
- The disc space and spinal canal is approached from the side. This allows the surgeon to perform the operation with minimal stretching of the nerve roots. The exposure of the spinal canal is done from one side only.
- The special spacer that is placed between the vertebrae helps restore the space between the vertebrae (the disc space). This can help reduce irritation and pressure on the nerve roots from bone spurs and thickened ligaments that can be a source of leg pain.
Preparations
Lumbar fusion may be indicated when conservative measures have failed to relieve low-back pain and there is significant disability and alteration of quality of life. Your spinal surgeon will gather a variety of information before recommending a spinal fusion. In addition to the history and physical exam, diagnostic studies can include standing spinal x-rays, flexion and extension x-rays to assess any spinal instability, MRI (magnetic resonance imaging) studies, myelogram or post-myelogram CAT scans, and/or lumbar discograms.
Once you and your surgeon have agreed that lumbar fusion is indicated, certain preparations for the surgery are important. You may need to donate one or two units of your own blood. This blood will be stored in the blood bank until surgery. If you need a transfusion either during or after your surgery you will receive your own blood back.
You should stop any anti-inflammatory medications 10 days prior to the surgery. You should stop smoking as soon as possible before surgery. This is very important to reduce complications from heart and lung problems. Smoking also decreases the success rate of fusions. Stopping smoking will increase your chance of a successful fusion. Your surgeon may have a brace made for you before surgery. This brace will be worn after surgery to support your spine and may increase the chance of fusion.
Discussions will be held with your family and people who may be assisting you once you return from the hospital. Some patients may require a short stay in a rehabilitation facility after leaving the hospital to recover from the surgery. You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition prior to the surgery. Hospitals often offer pre-operative teaching for patients undergoing major spinal operations. These teaching sessions can help you understand what to expect both while you are in the hospital and after you return home. A doctor who will be performing your anaesthesia (an "anaesthesiologist") will evaluate and counsel you regarding anaesthesia.
Procedure
Patients are usually placed face down on a special surgery frame. This position allows the doctor to operate on the back of the spine. It also lets the abdomen relax, which reduces blood loss during the procedure. General anaesthesia is used, meaning patients are asleep during surgery.
The surgeon begins by making a vertical incision over the section to be fused. Some doctors perform the TLIF surgery "percutaneously," meaning only two small openings are made in the skin.
The skin, muscles, and soft tissues are gently pulled aside. The doctor works through the main incision and separates the tissues over the back part of the iliac crest. A small amount of bone is taken from this part of the pelvis. The bone that is taken from the pelvis is prepared for use later in the TLIF procedure.
Preparations are made to insert pedicle screws. The surgeon watches on a fluoroscope (an X-ray that can be seen on a video screen) to determine the exact spot to place the screws. The screws are inserted through the pedicle bones of the vertebrae to be fused. For example, if two vertebrae need fusion, four screws are used, two on the left and two on the right.
The surgeon enlarges the opening around the nerve root, the foramen. An osteotome is used to cut the bone that surrounds this passageway. Enlarging the foramen takes pressure off the nerve root and gives the surgeon more room to do the TLIF surgery through the foramen. ("Transforaminal" means through the foramen). The nerve root going through the foramen is gently moved aside for the remainder of the TLIF procedure.
The disc between the two vertebrae to be fused is removed. The surgeon inserts a special surgical tool called a rongeur through the foramen and cuts a small "window" into the back of the disc. The disc is removed by working from the back toward the front of the disc space. When the disc and remaining fragments have been cleared away, the surgeon prepares the bony surfaces of the vertebral bodies where the disc was removed.
The surface of the vertebral body within the disc space is called the end plate. By peeling off the end plate with a curette, the surgeon causes bleeding to occur. The bleeding is needed to stimulate healing of the bone graft that will be placed into the interbody space.
The surgeon prepares to insert the spacer into the disc space between the vertebral bodies. The spacer, sometimes called a "fusion cage," is made either of bone, titanium, or carbon fibre reinforced polymer. Most are hollow so that bone graft material (taken from the pelvis or in the form of a bone substitute) can be packed inside the spacer. The surgeon measures the size of the disc space to ensure the best fit of the spacer.
Working through the foramen, the surgeon inserts bone graft material into the front half of the disc space. Next, a spacer is placed into the back half of the disc space and pushed as far as possible to the opposite side. A second spacer is inserted next to the first spacer. This completes the steps for fusing the front of the vertebrae (the anterior column).
Stabilizing the posterior column is completed by adding strips of bone graft along the side and the back of the vertebrae to be fused. Next, the surgeon realigns the surgery frame to give the low back a slight inward curve. Metal rods or plates are attached to the pedicle screws. Tightening this instrumentation compresses the vertebrae to be fused.
Complications
The potential benefits of spine fusion must be weighed against the potential complications of the operation. Thoroughly discuss the benefits and concerns of this major surgery with your surgeon, family, and family physician.
Complications can happen from anaesthesia, infection, blood loss (and possible transfusion), injury to the nerve roots, or hardware. The complications associated with this procedure could require a reoperation later. Medical complications are rare but may include pneumonia, heart attack, stroke, or blood clots.
While complications are not common, there are no guarantees that spinal fusion will be completely successful.
Afterward Hospital Course
Patients usually need to stay in the hospital for three to five days after TLIF surgery. An intravenous narcotic pain medicine is used to control pain for the first few days. Fluids are also given through the intravenous line.
A catheter will be placed in the bladder. Your blood counts are checked to determine if a blood transfusion is needed.
Patients begin a walking program the day after surgery. A physical therapist will usually schedule an appointment to help you learn to get out of bed and walking safely. You might even need a walker for the first few days. Your doctor may have you wear a back brace when you are up and about.
The surgical drain is usually removed within 48 hours of the operation, and patients can usually shower by this time. When patients go home, they are usually given a prescription for oral narcotic pain medication.
Rehabilitation
As mentioned earlier, some patients may need to stay temporarily in a rehabilitation setting before going home after being in the hospital. This brief stay involves intensive physical therapy to help patients get ready for a safe return home.
Pain varies in the first few weeks after spine fusion. You should expect soreness in your back. If your doctor used bone from your pelvis for the bone graft, you will probably have soreness in the spot where the bone was taken.
Pain from the surgery usually goes away in time, but no one should expect to have complete relief from spinal fusion. Some patients continue to have leg pain after surgery because the nerve was pulled aside during the TLIF procedure. Leg symptoms usually gradually improve. Be sure to follow your doctor's advice about taking prescribed pain medication.
You will schedule an appointment to see your spine surgeon within three weeks of the surgery. The doctor will look at the wound and talk to you about your progress. Notify your surgeon if you have a fever, wound drainage, or worsening of your symptoms at any time after surgery.
Upon returning home, you need to limit your activities for the first few weeks. You can get up to go back and forth to the bathroom. Avoid cooking, cleaning, driving or shopping at first. You are encouraged to continue the walking program you began in the hospital, as walking helps you heal.
Household activities can be gradually added to your routine after the first few weeks and as your symptoms allow. Getting back to work varies. Office work may be resumed six to eight weeks after surgery. Patients intending to get back to heavier work require a longer period of recovery. Many activities can be resumed four to six months after surgery. Most patients continue to report improvement in their symptoms up to one year after surgery.
Summary
Transformational Lumbar Interbody Fusion is a newer and effective method of fusing the lumbar spine. The goal is to improve back pain by stopping the irritation that causes mechanical and nerve pain. A successful result makes back symptoms better but not perfect. Most studies show that patients have about 60% improvement in their back and leg pain with TLIF surgery. More than 80% of patients who have TLIF surgery are satisfied with their surgery and recovery.
TLIF usually results in solid bone fusion with good pain improvement. However, there is no guarantee that the result will be successful.
TLIF surgery has advantages of increased fusion rate and decreased complications through a posterior approach. Spinal fusion is a salvage reconstructive procedure. No patient after a spinal fusion is 100% normal or 100% pain free. Complications do occur but are not common, and most patients are satisfied with their pain relief and the results of the surgery. It is critical that patients contemplating spinal fusion surgery are prepared both physically, as well as psychologically. All questions should be answered. Smoking should be stopped. This article has provided an overview only of this TLIF lumbar spinal fusion. Additional details should be reviewed with your surgeon so that all questions and concerns are discussed.
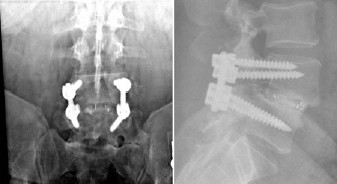
In these front and side views of a TLIF procedure, note the screws in the back of the vertebrae. The cage can only be seen by the white metal markers. Bone graft is in the disk space inside and around the cage.













