Cervical Radiculopathy: Surgical Treatment Options
This article provides information on surgery for cervical radiculopathy.
When symptoms of cervical radiculopathy persist, or worsen despite nonsurgical treatment, your doctor may recommend surgery.
The primary goal of surgery is to relieve your symptoms by decompressing, or relieving pressure on, the compressed nerves in your neck. Other goals of surgery include:
- Improving neck pain
- Maintaining stability of the spine
- Improving alignment of the spine
- Preserving range of motion in the neck
In most cases, surgery for cervical radiculopathy involves removing pieces of bone or soft tissue (such as a herniated disk)—or both. This relieves pressure by creating more space for the nerves to exit the spinal canal.
Surgical Procedures
There are three surgical procedures commonly performed to treat cervical radiculopathy.
They are:
- Anterior Cervical Discectomy and Fusion (ACDF)
- Artificial Disk Replacement (ADR)
- Posterior Cervical Laminoforaminotomy
The procedure your doctor recommends will depend on several factors--most importantly, the type and location of your problem. Other factors include:
- Your preference for a procedure
- Your doctor's preference and experience
- Your overall health and medical history (including whether you have had prior neck surgery)
Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is the most commonly performed procedure to treat cervical radiculopathy. The procedure involves removing the problematic disk or bone spurs and then stabilizing the spine through spinal fusion.
The goals of ACDF are to:

In ACDF, bone graft material is used to fill in the space left after the disk has been removed. Reproduced from Riew KD, McCulloch JA, Delamarter RB, An HS, Ahn NU: Microsurgery for degenerative conditions of the cervical spine. Instructional Course Lectures, vol. 52. Rosemont IL, American Academy of Orthopaedic Surgeons, 2003, pp. 497-508.
- Restore alignment of the spine
- Maintain the space available for the nerve roots to leave the spine
- Limit motion across the degenerated segment of the spine
Procedure. An "anterior" approach means that the doctor will approach your neck from the front. He or she will operate through a 3-5 cm incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.
During the procedure, your doctor will remove the problematic disk and any additional bone spurs, if necessary. The disk space is restored to the height it was prior to the disk wearing out. This makes more room for the nerves to leave the spine and aids in decompression.
Spinal fusion. After the disk space has been cleared out, your doctor will use spinal fusion to stabilize your spine. Spinal fusion is essentially a "welding" process. The basic idea is to fuse together the vertebrae so that they heal into a single, solid bone. Fusion eliminates motion between the degenerated vertebrae and takes away some spinal flexibility. The theory is that if the painful spine segments do not move, they should not hurt.
All spinal fusions use some type of bone material, called a bone graft, to help promote the fusion. The small pieces of bone are placed into the space left where the disk has been removed. Sometimes larger, solid pieces are used to provide immediate structural support to the vertebrae.
In some cases, the doctor may implant a metal, plastic, or bone spacer between the two adjoining vertebrae. This spacer, or "cage," usually contains bone graft material to allow a spinal fusion to occur between the two vertebrae.
After the bone graft is placed or the cage is inserted, your doctor will use metal screws, plates and rods to increase the rate of fusion and further stabilize the spine.

An anterior cervical diskectomy and fusion from the side (left) and front (right). Plates and screws are used to provide stability and increase the rate of fusion.
Bone graft sources. The bone graft will come from either your own bone (autograft) or from a donor (allograft) or it will be artificial bone graft. If an autograft is used, the bone is usually taken from your hip area. Harvesting the bone graft requires an additional incision during your surgery. It lengthens surgical time and may cause increased pain after the operation. Your doctor will talk to you about the advantages and disadvantages of using an autograft versus an allograft, as well as a traditional bone graft versus a cage.
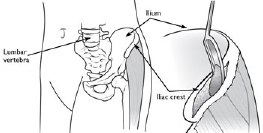
Most autografts are harvested from the iliac crest of the hip.
Artificial Disk Replacement (ADR)
This procedure involves removing the degenerated disk and replacing it with artificial parts, as is done in hip or knee replacement. The goal of disk replacement is to allow the spinal segment to keep some flexibility and maintain more normal motion.
Like ACDF, your doctor will use an "anterior" approach for the surgery—making a 3-5 cm incision along the neck crease. The exact location and length of your incision may vary depending on your specific condition.

Side and front view of patient with artificial disk replacement. Reproduced from Rihn JA, Lawrence J, Gates C, Harris E., Hilibrand AS: Adjacent segment disease after cervical spine fusion. Instructional Course Lectures, Vol. 58. Rosemont IL, American Academy of Orthopaedic Surgeons, 2009, pp. 747-756.
During the surgery, your doctor will remove your problematic disk and then insert an artificial disk implant into the disk space. The implant is made of all metal or metal and plastic. It is designed to maintain the motion between the vertebrae after the degenerated disk has been removed. The implant may help restore the height between the vertebrae and widen the passageway for the nerve roots to exit the spinal canal.
Although no longer considered a new technology, the development of ADR is more recent than that of ACDF. To date, the outcomes of ADR surgery are promising and are comparable to that of ACDF surgery. The long-term outcomes are still being researched.
ADR may be an option for you—depending on the type and location of your problem. Your doctor will talk with you about your options.
Posterior Cervical Laminoforaminotomy

In posterior cervical laminoforaminotomy, the doctor uses specialized instruments to thin down the lamina to gain better access to the nerve. Reproduced from Riew KD, McCulloch JA, Delamarter RB, An HS, Ahn NU: Microsurgery for degenerative conditions of the cervical spine. Instructional Course Lectures, Vol. 52. Rosemont IL, American Academy of Orthopaedic Surgeons, 2003, pp. 497-508.
"Posterior" refers to the back part of your body. In this procedure, the doctor will make a 3-5 cm incision along the midline of the back of the neck. The exact location and size of your scar may vary depending on your condition.
During a posterior cervical laminoforaminotomy, the doctor uses a burr and other specialized tools to thin down the lamina—the bony arch that forms the backside of the spinal canal. Removing this allows the doctor better access to the damaged nerve.
He or she then removes the bone, bone spurs, and tissues that are compressing the nerve root. If your compression is due to a herniated disk, your doctor will remove the portion of the disk that is compressing the nerve, as well.
Unlike ACDF, posterior cervical laminoforaminotomy does not require spinal fusion to stabilize the spine. Because of this, you will maintain better range of motion in your neck and your recovery will be quicker.
The procedure can be performed as open surgery, in which your doctor uses a single, larger incision to access your spine. It can also be done using a minimally invasive method, where several smaller incisions are made. Your doctor will discuss with you whether posterior cervical laminoforaminotomy is an option for you and, if so, how the surgery will be performed.
Complications
As with any surgical procedure, there are risks associated with cervical spine surgery. Possible complications can be related to the approach used, the bone graft, healing, and long-term changes. Before your surgery, your doctor will discuss each of the risks with you and will take specific measures to help avoid potential complications.
General Risks
The possible risks and complications for any cervical spine surgery include:
- Infection
- Bleeding
- Nerve injury
- Spinal cord injury
- Reaction to anaesthesia
- The need for additional surgery in the future
- Failure to relieve symptoms
- Tear of the sac covering the nerves (dural tear)
- Life-threatening medical problems, such as heart attack, lung complications, or stroke
Anterior Cervical Discectomy and Fusion and Artificial Disk Replacement Risks
There are additional potential risks and complications when an anterior approach is used in spine surgery. They include:
- Misplaced, broken, or loosened plates, screws, or implants
- Soreness or difficulty with swallowing
- Voice changes
- Breathing difficulty
- Injury to the oesophagus
- Pain at the site the bone was taken from—if an autograft is used
- Non-union of the spinal fusion (in ACDF)
Recovery
After surgery, you will typically stay in the hospital for 1 or 2 days. This will vary, however, depending on the type of surgery you have had and how many disk levels were involved.
Most patients can walk and eat on the first day after surgery. It is normal to have difficulty swallowing solid foods for a few weeks or have some hoarseness following anterior cervical spine surgery.
You may need to wear a soft or a rigid cervical collar at first. How long you should wear it will depend on the type of surgery you have had.
After spinal fusion, it may take from 6 to 12 months for the bone to become solid. Because of this, your doctor will give you specific restrictions for some time after your surgery. Right after your operation, your doctor may recommend only light activity, like walking. As you regain strength, you will be able to slowly increase your activity level.
Physical Therapy
Usually by 4 to 6 weeks, you can gradually begin to do range-of-motion and strengthening exercises. Your doctor may prescribe physical therapy during the recovery period to help you regain full function.
Return to Work
Most people can return to a desk job within a few days to a few weeks after surgery. They may be able to return to full activities by 3 to 4 months, depending on the procedure. For some people, healing may take longer.
Outcomes
Most patients experience favourable outcomes after surgery for cervical radiculopathy. In most cases, they experience relief from their pain and other symptoms and can successfully return to the activities of daily life after a period of recovery.













